Published in Ahram Weekly on November 12, 2012
As I go through the draft of the new Egyptian constitution, Article 11 strikes me as one of many curious articles in that supposedly foundational text: “The state protects the cultural, civilisational and linguistic unity of Egyptian society, and strives to Arabise science and knowledge.” Like others who have commented on the draft constitution, I have a problem with this article, but unlike others my problem is not that Arabising science might result in our doctors and engineers losing touch with the latest developments in medicine and engineering. Nor does my problem with this article stem from its failure to acknowledge or appreciate the complexity and diversity of Egyptian society.
Rather, my problem with it stems from two points. The first is my belief that much of the effort required for Arabising science has already been exerted. And the second is my conviction that this effort was exerted without paying much attention to such questions of identity as those that, I believe, lie behind the phrasing of this curious article.
I would like to share with you some thoughts on how science, and in particular medicine, was Arabised in the 19th century. Specifically, I want to relate the fascinating story of the founding of the Egyptian School of Medicine, aka Qasr Al-Aini, and the highly successful project of translating modern medicine into Arabic that the students of this school undertook, and which found its way to more than 100 superbly translated books published by the pioneering Bulaq Press. In telling this story, I will highlight the many problems that were encountered in the process, and will follow the efforts of the school founders and directors to overcome these problems. I would then like to take you with me into some of these books, so to speak, to appreciate the work done in rendering modern medicine into elegant, lucid Arabic. In particular, I will delve into two books, one on public hygiene and the other on anatomy, published in 1844 and 1848, respectively, and have a closer look at their structure, their argument, their audience and, above all, their language and the effort done in translating them. Finally, I will end with raising some questions about colonialism and identity.
***
Like many stories associated with modern Egypt, the story of translating science is related to the military. But, unlike them, it has a happy ending.
The story starts with Mohamed Ali’s desperate need to found an army to protect his power base in Egypt and prevent any attempt by the Ottoman sultan and his viziers to pluck him out of his prized province. In 1818, he therefore sent two expeditions to the Sudan to gather as many slaves as could be found and ship them down-river where they were sorted and screened for military service. The campaigns ended in utter failure: due to mismanagement, lack of proper transportation facilities, and above all lack of medical services, out of 20,000 slaves that were rounded up only 3,000 remained alive by the time they had crossed the huge distance to Egypt. The rest perished “like sheep with the rot”.
When he finally took the fateful decision to turn to Egyptians in 1821 to conscript them into the new army, he again encountered the same difficulty. Out of the thousands who had been gathered from their villages, hundreds were found to be too old, infirm or simply sick, and had to be sent back to their villages after enduring months of hardship.
Four years later, the need to found a medical corps for the new army was made abundantly clear to him by the repeated reports of high casualty figures among the soldiery. He therefore asked one of his European friends to secure for him a doctor who could found a reliable medical corps. In December 1824 one such doctor arrived in Cairo and proceeded to meet the pasha in the early months of 1825. This was Antoine Barthelemy Clot, who was appointed head of the army medical corps, hakimbashi al-gihadiya, and who would come to be known in Egypt as Clot Bey. (The pasha bestowed on him the title of “bey” to reward him for his heroic efforts in combating the devastating cholera epidemic of 1832).
Over a number of meetings with the pasha, the French doctor argued that, as experience had shown, the ravages of disease had more disastrous consequences for soldiers than wounds suffered on the battlefield, and that the best way to protect the new army was to found a local medical corps rather than solicit the services of European doctors. Towards this end, Dr Clot proposed to teach a nucleus of students in a newly constructed medical school that, in time, would supply the army with locally trained doctors, surgeons and pharmacists.
Crucially, Dr Clot advised Mohamed Ali that Arabic, rather than French, his own mother tongue, or Turkish, that of his patron, be used as the main language of instruction in the new school. He argued that for this new establishment to have any chance of success the doctors will need to be able to communicate clearly with their patients. This Mohamed Ali accepted and, in two years’ time, the new medical school was founded in Abu Zaabal to the northeast of Cairo where a large army camp had been located.
Immediately after the founding of the school and after the first batch of students had been chosen (incidentally, most were from Al-Azhar as this constituted the largest pool of literate young boys), Clot Bey encountered a serious problem. For he insisted that the new school’s curriculum should be founded on the latest medical theories and discoveries, and especially those of his compatriot Xavier Bichat, the famous anatomist and physiologist. Those doctors who were present in Egypt at the time, however, were mostly Italian physicians, whom he was determined to replace with his own countrymen, ending the privileged position of Italians and the Italian language in Egypt; or French quacks whom he thought gave both France and medicine a bad name.
Concurrent with his effort to select students, therefore, Clot Bey busied himself with recruiting French doctors to teach in his new school. Soon, however, two serious problems presented themselves and it is these two problems that I want to speak about in some details.
Both problems were about “translating science”. The first is the problem with the “metaphorical translation” of morbid anatomy that had to be based on dissection, and the supposed hostility this metaphorical translation elicited among Azhari scholars and the students alike. The second problem had to do with the “literal translation” of French medicine into Arabic, both orally and textually. As I hope will be abundantly clear, both endeavours met with spectacular success.
I do want to concentrate on the second problem, namely how the newly recruited French professors managed to communicate with the Arabic-speaking students, a problem that was made worse by the lack of Arabic medical textbooks they could use. However, I feel it is necessary to deal, albeit briefly, with the problem of “metaphorical translation”, i.e. how to overcome the religious sensibility against opening cadavers. This, I realise, is a separate topic altogether and one that warrants a separate lecture. Given that these two problems, that of the metaphorical and the literal translations of science, are interconnected, however, especially when it comes to one book on morbid anatomy that I want to discuss in some detail later on, I feel I should cover the first problem, the problem of overcoming the supposed hostility of Islam to dissection, before moving onto the literal translation of science in 19th-century Egypt.
No sooner had Clot convinced the pasha to set aside the necessary funds for what would be a long term investment than he encountered a serious problem. For when he wrote to the pasha telling him that the medical education he had in mind would be squarely based on dissecting human cadavers, he received a firm reply that cadavers were not to be touched. In his Mémoires Clot explains how, undeterred, he managed to overcome this formidable barrier:
“I harboured the hope that one day I would vanquish this prejudice even though I clearly noted the profound disgust of the students and the fanatical opposition of the ulémas [sic.] with whom I had had communication on the subject. I applied myself to winning the confidence of Cheikh El Islam al-Arusi, an important person who enjoyed a high reputation for holiness in the country…. When I approached the question of anatomy he would not give a single concession. His principal argument was that, according to religion, cadavers could feel pain, to which I concurred, but added that bodies would decompose and become the prey of worms soon after death [anyway]… [The Sheikh then argued that medical treatises] published on such subjects should suffice for the instruction of the students… [I responded] that the theory provides no more than incomplete notions: a watchmaker, I told him, who has to repair watches, does he not need to understand their whole mechanism? Moreover, does he not have to put together and take apart the various pieces before he can understand how they operate? This image struck him… [and] I managed to obtain a tacit agreement to study anatomy but to act with the greatest discretion and to do so in secret.”
It is clear that Clot is referring here to the theory of natural theology which argues that design implies a designer. This theory had become famous in England in 1802 with the publication of William Paley’s book simply titled Natural Philosophy, in which he used the watchmaker analogy. This book was translated into French the following year, 1803. Clot may have read the French translation, but it is difficult to be certain about this point.
Be that as it may, in his Mémoires, published by the IFAO in 1949, Clot describes how, having received the tacit approval of the ulama, he proceeded to deal with the prejudices of the students. After placating them by promising that he would never apply the scalpel to a Muslim’s body and that they would only work on the bodies of Negro soldiers, work progressed slowly and cautiously on learning descriptive anatomy and the first dissection lesson was conducted in 1829.
Then, on 20 June 1829, while watching the physiology lesson of a colleague, Clot was attacked by a student with a knife in his hand; only by an instinctive move of his arm did he manage to avoid a fatal wound. The attacker was immediately grabbed and disarmed, and Clot ordered him detained in the hospital’s jail. But the incident left Clot completely demoralised. “I admit that from the time I was hit by the young fanatic man a deep despondency seized me… Sacrificing one’s life, giving up one’s peace in order to conquer the prejudices of a people, to develop their intelligence, to extend to them the benefits of civilization only to be rewarded by indifference, if not hatred, this thought overwhelmed my soul.”

In the Museum of Medical History, in the old Qasr Al-Aini Hospital on Roda Island, hangs an interesting painting that depicts the first anatomy lesson conducted in Egypt. While it does not depict the attempt on Clot Bey’s life, I read this interesting painting as effectively an illustration of Clot Bey’s Mémoires and his self-image as a determined prophet of Enlightenment.
In addition to the curious Arabic inscription, the meaning of which I will come back to later, it is interesting to note Clot Bey’s position as well as the position of the guards at the entrance of the amphitheater as well as the absence of a text.
Typically, European dissection paintings contain a text that is being read aloud by the lector (as opposed to the sector), in a clear reference to the dialogue that characterised anatomy lessons in such places as Padua, Paris and Edinburgh: Simply put, this dialogue was over which has precedence over the other: the text or the cadaver? Is the corpus of medical literature that glossed over Aristotle and Avicenna to be discarded in favour of direct observation of the dissected cadaver, or does the corpse only corroborate the teachings of the ancients? As late as Rembrandt’s 1632 Anatomy Lesson of Dr Tulp, we see such a reference to this tense dialogue.
In our painting, we do not see this tension between body and text — at least not explicitly. However, the way the artist placed the ulama, the custodians of the text, in a position that obstructs visual access to the cadaver by both students and us, spectators, the ultimate source of medical knowledge, is, I think, a fair reflection of Clot Bey’s self-image as a prophet of the Enlightenment, determined with his rational thinking to combat superstition, religion and magic.
Before moving onto the second problem, that of trying to find a common language between doctors and patients, let me briefly say that for the past 15 years I was intrigued by the question of whether or not one can describe the medicine that Clot Bey introduced in Qasr Al-Aini as “colonial”, a question that necessitated that I probe deeper into the issue of “translation” between “Islam” and “modernity” as illustrated by the tense practice of dissection.
As I said earlier, this is a question that warrants a separate lecture, but let me say briefly that I believe Clot Bey’s position regarding this question was a complex one, a position that is expressed differently in different publications: there is a marked difference between what he says in his French books, intended for a Western audience, what he says in his Arabic books, translated by his own colleagues and students and addressed to his students, his subordinates and the wider public, and what he says in the numerous unpublished journals of the many medical bodies he headed, documents that are now housed in the National Archives.
Let me also add that in order to see whether Clot Bey’s watchmaker analogy was aimed at Muslim clerics in particular (as many of his subsequent Egyptian translators and publishers — most importantly Gamaleddin Al-Shayal, Naguib Mahfouz (the gynaecologist, not the novelist) and Jaques Tagher — seem to think) or whether it derived from a more general anti-clerical attitude that many post-revolutionary French thinkers adopted, I conducted some research in the National Archives on the position of “Islam” vis-à-vis dissection.
My research was aimed at discovering what the clergy had to say, what classical fiqh had to say, what the doctors (themselves former Azhari students) had to say, and what patients had to say. While I am going to touch upon the position of the students towards what they had been learning and especially dissection, let me say briefly that I found no evidence that subaltern Egyptians were opposed to dissection in principle. While the archives contain numerous references to incidents in which people were opposed to post-mortem examinations, in general, and to autopsies, in particular, police records are also replete with cases in which it was the relatives of the deceased who insisted on an autopsy.
Like Khaled Said’s family and that of Essam Atta, the first anniversary of whose death is these days, 19th-century Egyptians realised soon after the introduction of dissection in Qasr Al-Aini how important this new practice could be in proving legal cases against strong men who had beaten or tortured to death their loved ones. Lacking eyewitnesses or confessions, the two principal means of establishing proof in the Sharia court, Egyptians were only too willing to ask for their loved ones to be dissected if this was the only means to prove that theirs was an unnatural death. And this they did without thinking that they were contradicting their religious convictions or violating the sanctity of the body called for by Islam. Their insistence on justice trumped the blind observance of burial rituals that Clot Bey’s Mémoires depicted as a serious problem preventing modern medicine from being translated in Egypt.
***
Now, to move to the second problem encountered in founding Qasr Al-Aini, namely the problem of literally and not only metaphorically translating medicine, one can easily see how this was the more difficult of the two. To remind you, Clot Bey insisted that the young doctors should receive their education in Arabic. However, none of the European doctors knew Arabic (they were mostly French, but there were some Italians and one Spaniard too). At the same time, none of the students knew French, as that language was not, and still isn’t, part of the curriculum of the Azhari schools. At the same time, there were no Arabic books on modern medicine that the Qasr Al-Aini professors could teach. The way Qasr Al-Aini managed to overcome this problem is truly remarkable and the resulting effort of translating nearly 100 books in all fields of medicine from anatomy to obstetrics, and from surgery to public hygiene, deserves a privileged place in the annals of translation into Arabic, and indeed in the annals of translation.
For a while, Mohamed Ali flirted with the idea of ordering the newly arrived doctors to learn Arabic, and to deny them any assistance from government translators a year after their arrival in the country. Upon hearing this, many of those professors rebelled, saying that they came to Egypt to teach medicine — not to learn Arabic. For his part, Clot had been trying out a process that looks cumbersome and inefficient; but, lacking any other means, he insisted on it until a nucleus of bilingual students could be formed. This cumbersome process entailed the following:
First, the professors would deliver their lectures to a handful of translators and make an extra effort to explain the content of the lecture, paragraph by paragraph. The translator would then write down his Arabic translation in a copy book.
Second, the translator would translate back to French what he had written in Arabic. This way, the professor would make sure that the translator had truly got the meaning of the lecture.
Third, the Arabic translation would then be delivered by the translator to the students in their classrooms.
Fourth, the professor would then deliver the lecture through the translator to the students and answer any questions they may have.
Fifth, at the end of every month, students would be examined in what they had learned through this cumbersome process.
(I have a hunch that this was the main reason students tried to kill Clot Bey).
The problems involved in this process of teaching medicine were clear for all to see; not least, the Qasr Al-Aini faculty themselves. And they wrote to the Schools Department, which was in charge of all polytechnics in the country, to complain of wasted time and energy. For his part, Clot Bey was aware of the many problems inherent in this process, and he was striving to find a long-term solution to it. The problem so far was that the translators who were around at that time, i.e., in the late 1820s were few and far between and, naturally, not well versed in medicine, if at all. Most, if not all, of this first generation of translators were Maronite Christian Syrians who had been residing in Egypt since the 18th century, and who knew either French or Italian.
A long-term solution had to be found; and one has to admit that Clot Bey’s multi-pronged approach was ingenious: First, he ordered the group of Syrian translators to get together and start working on translating not only the oral lectures but a handful of textbooks. The first medical book to be translated was an anatomy book which appeared in 1832 called The Frank Statement on the Science of Anatomy. The translator was a Syrian translator by the name of Youhanna Anhuri, who was a descendant of an old Syrian family (from ain hur, hence the name). Interestingly, Anhuri knew only Italian; and this book, together with the six other books he translated (one in pathology, two in surgery, one in public hygiene, one in physics and one in botany) had to be translated first from French to Italian so that he could then translate them from Italian to Arabic.
Other Syrian translators included George Vidal, a Maronite Syrian from Aleppo (who, according to a certain baptismal record kept with the Fransiscan Friars in Cairo, might have been baptised in 1795) who translated a book that I will mention in some detail later on, and August Sakakini from the famous Sakakini family, who would later translate many of Clot Bey’s medical treatises that were intended for army doctors and government schools.
As has been said, these translators had already been translating the oral lectures of the Qasr Al-Aini faculty; in time, they came to acquire a lot of the medical knowledge of the subjects they were translating. Indeed, by the late 1840s they had become experts in translating medicine.
No sooner had this problem been solved, however, than another problem presented itself. Given their Christian background, none of these Syrian translators knew the Quran, and hence their Arabic language left much to be desired. To solve this problem, Clot and his patron, Mohamed Ali, deployed their third tactic to improve the quality of translation, namely, to appoint a number of Azhari sheikhs as editors and proofreaders of these books. With their mastery of Arabic, and apparently with their knowledge of mediaeval Avicennean medical lore, these Azhari translators not only managed to render the translated texts into lucid Arabic; they also managed to supply the translators and the authors themselves (for many of these early books were authored by the Qasr Al-Aini staff) with Avicennean medical vocabulary. As we will see, some of the French concepts and terms written in the original books were themselves derived from mediaeval Latin, which in turn was mostly derived from Avicenna’s Canon, Al-Qanun fil Tibb.
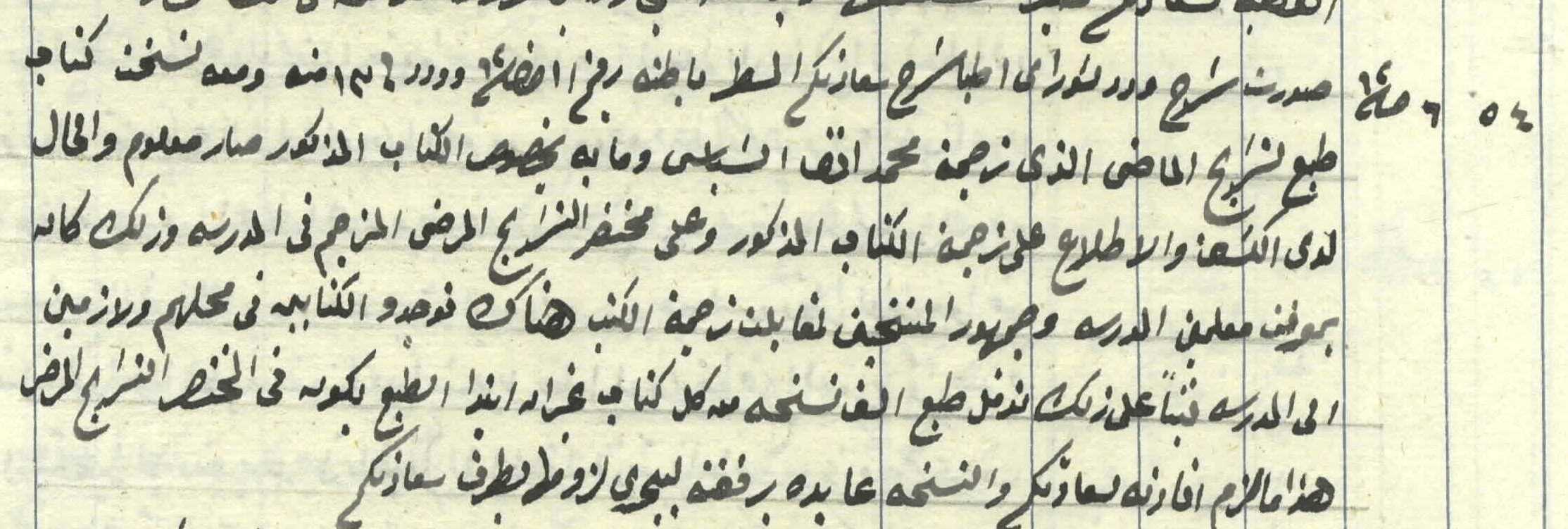
One of those Azhari editors of Arabic deserves special mention. His name was Mohamed Al-Harrawi, and he was the chief editor, i.e. Arabic language corrector, of the first 250 or so medical books that Bulaq printed. For a while, it seems that he was in charge of an ill-fated preparatory school that was founded in the early 1830s to prepare students for the medical school itself. However, Clot Bey did not believe that this school was doing a good job (this was the symptomatic of a general government neglect of preparatory schools), and some tension developed between him and Harrawi, a tension that required Mohamed Ali to interfere in person, and to remind Harrawi that his position was an editor and nothing more.
Two other Arabic editors deserve special mention. Both have the same last name, Al-Rashidi, although they were not related. The first was called Ahmed Hassan Al-Rashidi and the second was Hassan Ghanim Al-Rashidi. Both were Azhari sheikhs who had been recruited to the medical school as editors of Arabic, and the first, Ahmed Hassan, was the editor, together with Al-Harrawi, of the first medical book, The Frank Statement on the Science of Anatomy, that had been translated by Anhuri and which had appeared in 1832. Given the expertise that they had acquired in editing medical books, they were both chosen by Clot Bey to join the first medical student mission that he sent to France in 1832. They both returned six years later, in 1836, and were appointed professors in Qasr Al-Aini and became translators in their own right.
This, then, was the fourth long-term method that Clot Bey employed to overcome the problems of translation, i.e. sending a limited number of Qasr Al-Aini graduates to Paris to continue their education and to translate one major book in their field of medical specialisation as condition for gaining government employment on their return. I will have occasion to talk about one of these students, Mohamed Al-Shabasi, in a minute.
Using this multi-pronged approach, Qasr Al-Aini was able by the late 1840s, i.e. less than 25 years after it was founded, to have a well-rounded mini-library of some 50 medical titles that had been translated into a legible, correct and lucid Arabic. These titles covered most fields of medicine known at the time. This included morbid anatomy, pathology, gynaecology, paediatrics, pharmacology, public hygiene, osteology and ophthalmology.
The students who graduated from Qasr Al-Aini, whose records I follow in Dar Al-Wathaiq, were therefore fluent in Arabic, while at the same time intimately cognizant of French, some even fluent in it. The language of instruction, however, as well as of general correspondence of all medical bodies in Egypt, and there were many, remained Arabic. And, as said above, it was a fluent, correct Arabic, thanks, in no small part, to the efforts of the Azhari proofreaders in Qasr Al-Aini.
I want to conclude with some remarks about the actual content of these books, both in style and in substance.
Let me start with style.
Most every one of these books had a rhymed title along the lines of mediaeval Arabic medical books. This rhyming style was mostly the work of the Azhari copy-editors, and their play with words exceeded the titles and included the sometimes lengthy introductions that they wrote for the books.
Second, in addition to its rhyming language, every single introduction to these books waxes poetic on Mohamed Ali and his efforts to resurrect the science of medicine in Egypt. Most interestingly, Mohamed Ali, and occasionally Clot Bey, are praised in light of the fact that “resurrecting” science, which had once thrived in Egypt and in Arabic, had long since disappeared. In none of the books I read, and I repeat, in none of these books, is Mohamed Ali or Clot Bey praised for attempting to “translate” Western science into Arabic. In none of them is this amazing effort of translation seen as an attempt to “catch up with the west” or to “borrow from the West”. In fact this whole civilisational language, this whole discourse of clash of civilisations, is conspicuously absent from this phenomenal effort. There is no anxiety about identity or concern about provenance that can be detected in the works of this generation of doctors, administrators, editors and translators.
In terms of substance, one can detect this same degree of self-confidence and self-pride in what these doctors/translators were saying. Let me illustrate this by two examples.

Al-Shabasi’s Al-Tanwir fi Ilm Al-Tahdir): This was an Azhari student when he joined the Qasr Al-Aini school in 1827, and joined the first student mission to France that was dispatched in 1832. He stayed in France till 1838 (or 1840). On his return to Egypt he was appointed professor of physiology and pathological anatomy, the most prestigious of academic positions at the Qasr Al-Aini School of Medicine; in the adjoining hospital, he was put in charge of the Venereal Disease Clinic. The first work translated was Jean Cruveilhier’s Anatomie pathologique du corps humain, (two volumes, 1829-1840) which appeared in Arabic under the title of Al-Tanqih Al-Wahid fil Tashrih Al-Khass Al-Jadid. In addition, he wrote this one-volume textbook, Al-Tanwir fi Ilm Al-Tahdir, as an aid for his students on how to prepare corpses for autopsy and how to conduct the autopsy itself. It was this latter work that was the basis of his fame. Al-Tanwir was presented to the Health Council, which ordered 1,000 copies to be printed. If we are to believe what the author says of the book’s effects on his students, it appears to have been a smashing success: students were in the habit of taking corpses to their lodgings to learn more about human anatomy and they had no problems sleeping in rooms where dead bodies were kept, heedless of the criticism that this triggered.
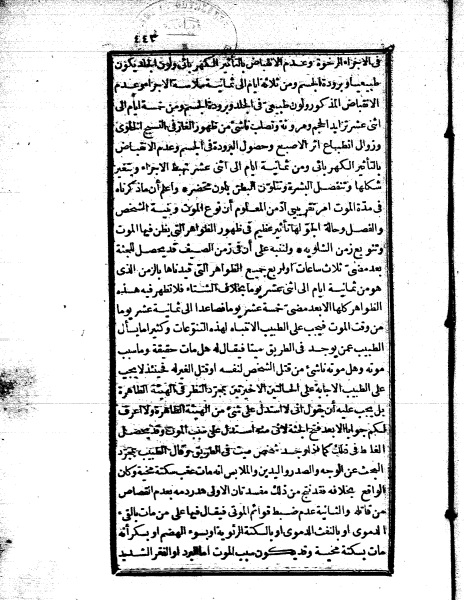
In the preface to this second book, Al-Shabasi states explicitly that “it is common knowledge among civilised nations that medicine cannot advance except by practising dissection. Opening cadavers,” he adds, “has many benefits. Among them are acquiring the knowledge of how the healthy organs might have looked like just before death. It also enables us to identify pathological transformations that affect each organ and to compare them to symptoms detected just before death, and thus helps us diagnose illness [in similar situations]. It can also be useful in problems related to forensic medicine such as burns, poisoning, homicide, drowning, falling [from a high place], or dangerous wounds. Moreover, it can be of use in pointing out dangers that should be avoided while conducting small or major surgical operations.” Adding to these “scientific” benefits, Al-Shabasi finds no problem in adding another “religious” one, which is “marvelling at the precise functioning of the organs and meditating on God’s creatures, which deepens and strengthens one’s faith.” He then quotes Galen: “Reading anatomy books is the greatest of all acts of worship and it forces one to acknowledge God’s oneness.”
Throughout his book Al-Shabasi sees no contradiction between his background as a graduate of Al-Azhar or his personal faith, on the one hand, and his profession as a medical doctor and a professor of physiology and pathological anatomy, on the other. This harmonious view of his Islam and modern medicine is seen most clearly in the conclusion of his book, where he dwells on the importance of dissection for forensic medicine:
“What we have just explained should enable the forensic doctor to be sufficiently alert so that he can distinguish between apparent death and real, clinical death. [Another value of dissection can be illustrated by] the example of three people who had drowned at the same time. As a result a problem of [Islamic] inheritance arises, a problem that could only be resolved if we determine who died first. Specifically, one person could have died as a result of a stroke, the second died by fainting [sic.] and the third struggled with drowning for some time and eventually died of asphyxiation. In this case the forensic doctor could deduce from the condition of the arteries, the veins, the heart, the lungs, etc. certain rational conclusions based not on guesswork, but on visually checking [these organs]. The same could be said in other similar cases, as when many people die at the same time in an earthquake, the collapse of a building, or a fire. [In all these cases the forensic doctor] must be careful to make clear that his results are not absolute truths, but only approximations to the truth.”
In his very last remark, Al-Shabasi reminds his students of the importance of diligence in their work and cautions them not to jump to easy conclusions.
“When the forensic doctor comes across a dead body in the street, he should be very careful how to identify the cause of death. For if he says that the victim died as a result of a brain stroke [i.e. a natural death, when in fact] death was caused otherwise [i.e. unnaturally], then two errors are committed: first the Sharia-stipulated capital punishment, qisas, [i.e. talion, retaliation] from his murderer is prevented, and, second, this case would be recorded wrongly in the death registers.”
The ease by which this former Azhari student who occupied the chair of professor of physiology and pathological anatomy in Qasr Al-Aini could combine his understanding of Islam with his belief in the value of human dissection is a far cry from Clot Bey’s assertion that “religious superstitions” hampered his work in Egypt. In this remarkable book, which is written in a non-polemical, matter-of-fact style, and which was intended not for the general public but for medical students, Al-Shabasi clearly explains how dissection could be of aid not only to medical education, but also to the proper collection of vital statistics and, what is most remarkable, to upholding the Islamic principle of retaliation for a medically proven case of homicide.

I want to end with another amazing book, Kunuz Al-Sihha wa Yawaqit Al-Mihna. This is a book on public hygiene written by Clot Bey not as a textbook to be used for the Qasr Al-Aini School, but for the general public. The book was translated by Mohamed Al-Shafei, and edited by two interesting figures that I want to say something about, Mohamed Omar Al-Tunisi and Dr Nicolas Perron.
Kunuz Al-Sihha was first published in 1844 in 1,000 copies. Due to its popularity, it was printed again in 1849, then a third time in 1854, then for a fourth time in 1878, all in Bulaq. As proof of its immense popularity it went into commercial publications, first in 1884 when the Sharaf Press published it, then in 1886 when it was printed by Abdel-Razek Press and in 1903 by the Yemini Press. What was the secret for the success of this book on public hygiene?
Well, for one thing, it was written in a very clear, matter-of-fact, simple language addressing the average person. It is not condescending, nor patronising. For another, it has a lot of interesting new useful medical information without at the same time claiming to be a guide for self-medication.
Mostly, I think the success of the book lies in its translation. And I don’t mean the ability of the translator to find suitable Arabic words for what was a state-of-the-arts medical book on public hygiene, nor the ability of the editor to render this final product into lucid Arabic. Rather, I mean that the book does not appear to have been translated. I am not familiar with translation studies jargon, but I am sure there is a word for this school of translation in which the final product reads seamlessly.
Let me give some examples:
The book starts with a 15-page excerpt from Makrizi’s Khitat, specifically the section in which the famous chronicler speaks about the bimaristans of Cairo’s. The intention was clearly to situate Qasr Al-Aini within a long, indigenous tradition of health care and hospitalisation. The book also makes occasional reference to classical Arabic poetry, most notably comparing untrained medical quacks with the blundering of a blind camel (khabt ashwa), in a clear reference to Zuhair’s famous muallaqa: “I see death is like the blundering of a blind camel;… him whom he meets he kills, and he whom he misses lives and will become old.”
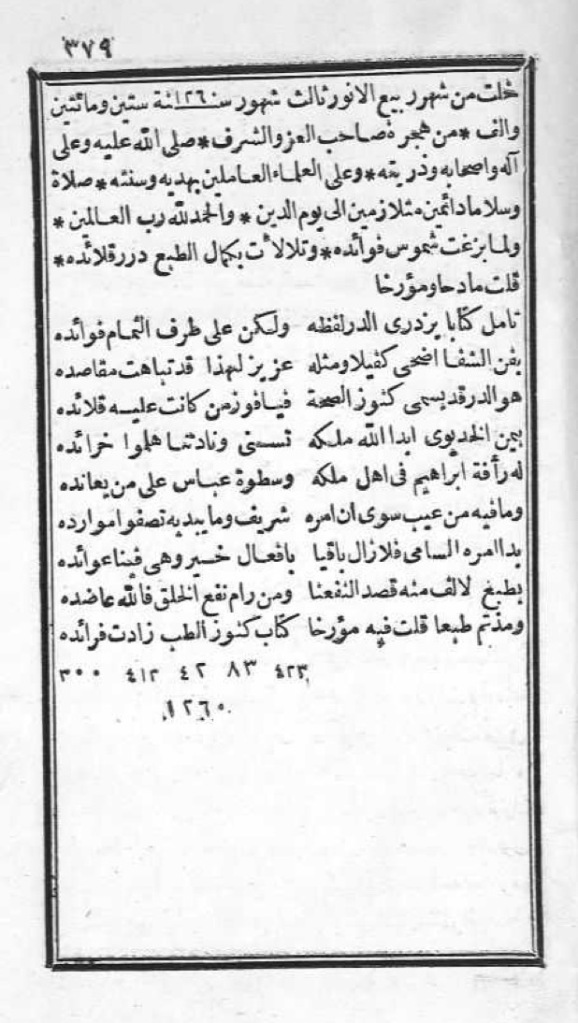
And, finally, there is the chronogram with which the book ends. Chronograms are an extinct art form, once very popular among Cairene (and other Ottoman) literati, that plays on the numerical equivalence of the letters of the Arabic alphabet to end up with a figure that corresponds to a date with which an event is dated, which is here, 1260 the Hijri year of publication.
This “translation” is the result of collaborative work of four amazing people, whose lives — each on its own and taken together — illustrate what was truly impressive about this effort of translating science in 19th-century Egypt. First, there is Clot Bey himself, an amazing teacher and physician in his own right, but also a superb politician and administrator. An incisive judge of character and someone with a witty tongue and scathing sense of humour, he managed to put together an impressive team in his school and to succeed in his mammoth task against all odds.
Then we have Mohamed Al-Shafei, one of Clot Bey’s students, who was originally an Azhari student, joined Qasr Al-Aini when it first opened in 1827, went to France on the 1832 student mission, returned in 1838 and was appointed professor of internal medicine in the school. In 1840 he was appointed director of the School of Midwives, and in 1845 deputy director of the Qasr Al-Aini School of Medicine. He translated three books; this is one of them.
The third man is Nicolas Perron, professor of chemistry at Qasr Al-Aini. Perron is one of the most amazing figures in this whole enterprise, as he was the only one of the Qasr Al-Aini faculty who mastered Arabic and who could speak, read and write it fluently. In fact, he can be considered to be a leading Orientalist in his own right. He had arrived in Egypt in 1827 after studying with the famous French Orientalist, Silvestre de Sacy. He taught for many years in Qasr Al-Aini until he became its director after Duvigneau (1839). He died in 1875. He was an avid reader of the classics of Arabic literature including Al-Aghani of Asfahani, and he made a huge effort in translating into French Al-Qamous Al-Muhit, Firozabadi’s dictionary, just at the time that Lane was doing the same but into English.
The fourth person is Mohamed Ibn Omar Al-Tunisi, who was one of two Azhari sheikhs that Perron befriended and respected. Sheikh Mohamed’s father was originally from Tunisia, but had resided in Sudan. Mohamed joined Al-Azhar and then went to seek his father in the Sudan. He ended up writing two books in Arabic about his trip to the Sudan, which Perron helped him publish in France. Mohamed returned to Egypt and joined Mohamed Ali’s, first as an imam in the army, then in Qasr Al-Aini where he met Perron and started reading with him Kalila wa Dimna in Arabic.
These are the four men who together wrote and translated this impressive book, Kunuz Al-Sihha. They are an amazing group of men. Each grew up in one place and ended up in another. All were well travelled, well read and self-adjusted. Clot Bey was a physician from Marseilles who came to Egypt to found a medical school to teach in Arabic. Shafiaa was an Azhari student who joined the Qasr Al-Aini Medical school, went to Paris to continue his education and returned to Egypt to teach and then head the school. Perron was a French chemist who fell in love with Arabic, came to Cairo, taught at Qasr Al-Aini, befriended many Azhari sheikhs, and ended up editing tomes of classical Arabic literature. And Tunisi, one of those Azhari sheikhs that Perron respected, was, as his name indicates, from Tunisia, grew up in Sudan, entered Al-Azhar and then busied himself with editing medical books in Qasr Al-Aini.
Together, these men and many others helped translate modern medicine into lucid Arabic in what could be rightly regarded as a truly impressive effort at translation and mediation. None of them was motivated by an effort to “enlighten the ignorant” masses the way we find in many colonial situations, and none of them thought of his project as that of attempting to catch up with the west or even as borrowing from the West. For them, science was science; it knew no provenance and did not belong to any particular nation.
Arabising science back then had nothing to do with identity and was not informed by any attempt to restore an injured psyche. Rather, translating medicine was a creative endeavour that allowed these men an opportunity to engage in cutting-edge science and to end up participating in an intellectual activity that saw no hermetic boundaries between languages and/or cultures.
Lecture delivered in the Oriental Hall, AUC on Monday, 5 November 2012.
